Introduction
Too often leadership is understood to be something that chief executives, directors or senior managers do, assuming a degree of ‘command and control’ or a body of followers.
The truth is that we need leadership at all levels of the social services workforce, and from the people they support, to deliver better outcomes. This is about workers ‘doing with and not to’, truly listening and stepping up or stepping back as required. This requires them to be a champion and advocate at times, and at other times, remember that people are experts in their own lives and support their leadership. What matters to them is central.
It’s also about knowing yourself – being true to your values and letting that be your guide in times of uncertainty, and knowing when to reach out to others for help. It’s about self-reflection and thinking about what you can do better next time.
Leadership requires working in partnership with other professionals too - and in the in-between spaces this creates. It can challenge traditional, more hierarchical ways of working, ‘tick box’ approaches and requires people to value one another.
The following stories beautifully illustrate what everyday leadership looks like from the frontline - and the difference it can make to the lives of people that are supported. They provide inspiration, and identify some of the challenges that those ‘at the top’ need to understand too.
A massive thank you to Leeann Davidson, Jenna Scott, Carolann Neish and Claire McAllister for sharing their stories, and to their lecturers, Helen Rainey and Elaine Gifford, on the BA (Hons) in Integrated Health and Social Care at the University of the West of Scotland.
This work contributes to a national programme on leadership led by the SSSC. If you want to explore this topic further, go to Step into Leadership where they identify six leadership capabilities. You can also explore this leadership logic model, which shows how leadership contributes to positive outcomes.
How to use these stories
Read Lee, Jenna, Carolann and Claire’s stories and ask yourself:
As leaders…
- What do they bring of themselves?
- What do they do and how do they engage?
- How do others respond?
- What enablers do they experience?
- What challenges do they experience?
- What difference does it make?
- to those they support?
- to their organisation or peers?
- to their sense of self?
Lee's story
I ended up on this course (BA in Integrated Health and Social Care at UWS) by accident - as a care experienced person my aspirations didn’t quite get me to university. It was by accident and I’m really glad I did it.
I'm also a Mindfulness and Wellbeing Coach. I volunteer in the community in three different organisations, delivering mindfulness classes. I’ve been running these for three years. I started them as a student in my placement cos I sought out Shelter Scotland for my placement in my HNC year and I’ve been running the groups since then. I think I’m on group number 18 or something like that now. And I've made it onto the Board of Directors with Who Cares Scotland. (The Board is responsible for its strategic objectives and financial oversight, and it includes at least five people with care experience.)
I was informed by my own lived experience of homelessness, recognising the need for mental health support in the group. During homelessness you’re picked up and put away somewhere else and it makes it difficult to integrate into the community. Loneliness and isolation is one of the biggest things for poor mental health, so using my lived experience I recognised the need in the organisation I was in.
To recruit a group, I went looking for them and met them face to face. They were service users and I met them all personally, had a cup of tea and a chat to build up the relationship. I met them about four or five times before the group started. I work with a relationship-based approach all the time. I think it’s better for somebody to know the person behind the organisation, otherwise you can’t get someone to come to a group. Group therapy is hard for everybody, but getting people to come and initiate and participate in a group is quite difficult, so if they know the person that they’re coming to, they are more likely to engage.
Just coming along to the first group was the major hurdle for a lot of them, as a lot of them were staying in the house. The only time they would come out is when they were meeting their befriender and that would be the only time they would come out of their house - it was their comfort zone. I was a different befriender so I needed to build that up so they knew who they were coming to see.
On the first day of the mindfulness group it was really just about getting it off to a good start, I think, and putting the right things in place. Then a lot of it’s really around getting everyone to gel together. It’s more about me facilitating them to support each other - having them lead the group. It’s about what they want to learn as opposed to me telling them what to do.
The first one was quite successful. Everyone I invited turned up, so I ended up with 14 service users that day which was terrifying at the same time! Do you know when people say, ‘Yeah, I’m coming along to the group.’ You just think, they’re being nice and they’re just saying yes to you at the time, so I kind of panicked but it was a good panic.
I started with ice breakers where I led the conversation. I told them a wee bit about myself - I related to them in a sense that I knew where they are at, cos I knew what homelessness was. I had been there. I tended to share a wee bit about myself ... so that made them feel like I was not just there doing a job. Being a volunteer gives you that unique position where people relate to you a wee bit better cos it isn’t just a job for you. I introduced what mindfulness was, asking if any of them had had experience of what mindfulness was?
I provided lunch which was great because that’s always a good ice breaker for people too.
I did the emotional check-in at the beginning and the emotional check-out at the end just to see how everybody was feeling. I made sure everyone was safe when they were leaving and stuff because during the group there was quite a lot of information shared. I think it was a collective sigh of relief for everybody where they suddenly realised that they’re not on their own. It’s all kind of similar feelings and issues that they were all facing cos they were all in similar situations, so that sort of solidarity around the problems they were facing was them helping each other as well.
I speak to service users the same way that I would speak to my friends, which makes me more relatable. In the evaluation sheets at the end they all said that it was just like being with one of their friends, that they were able to come and relax and have a cup of tea with and just offload, and that made things much easier for them. I think me being as accessible and relatable by building up the relationship meant that they felt more comfortable as well.
The first one was just a chillax group, somewhere to come and just have a cup of tea. Then it developed where they were wanting to cover more serious issues, I suppose, rather than just being able to take care of themselves. I adapted the service to suit them because there’s no point me delivering the same thing if it’s not what they’re needing, so they actually co-produced what I do now. For instance, we’re currently covering social anxiety - a lot of people were saying that they struggle with going outside so I tailor it to them cos there’s no point me just teaching mindfulness all the time if that’s not what they’re needing.
Now I have another volunteer who is a trainee CBT therapist, so we’re covering two different sorts of things and ever-adapting the group to whatever they need. We cover different issues each time cos I run it in six week blocks and I stop over the school holidays. Childcare was one of the barriers for people and that was identified quite early on, so we changed the class to a Wednesday when the kids were in school and it was at lunchtime. It finished in time for everybody to go to collect their kids cos we couldn’t provide a childcare facility as we don’t have the funds for that. Running the group costs £4000 a year just on lunches. We managed to get the hall for free which was great.
They all come for their lunch and a cup of tea! That’s probably the bit they look forward to the most and all the fidget things that I get for the group cos I tend to put lots of fidget stuff on the table and hand creams and stuff like that.
That’s me in my third year now....
One of the things that the service users keep telling me is that there just isn’t enough community things going on that can support poor mental health in the community. This is because accessing mental health services is really difficult, especially in Renfrewshire.
The need is there, everybody needs these kinds of things and the fact that I’ve got a core group every single week of at least 10 people shows you that the need is there for that. Even organisations are approaching and asking, ‘Can you come in and do it with our staff because we need that.’ Just somebody to talk to, a sounding board - someone who is not quite as difficult to get a hold of in comparison to mental health services.
A lot of the evaluations that I collect tell me that they take things home and they’re calmer. They use some of my techniques. Everyone does their homework as well which is awesome because I don’t even like doing homework! But everyone does their tasks that I set them and things like creating a mood board for themselves, so that when they’re having a down day and stuff like that they’ve got that there to remind them who they are and what they’re doing and why they’re doing it. They tell me that they’ve done it. They even show me pictures of their mood boards.
One particular service user started one of my groups - she did 12 weeks. When she first came in she had her hair down, she spoke to the floor and she didn’t really join in the group or anything like that. She was really quiet, shy and anxious, and she was always using the fidget things and the hand creams and going to the bathroom a lot. She was finding it really difficult to be in the group. By the end of the 12 weeks she had enlisted in volunteering to help children. She had her hair in a ponytail and she was really happy to talk. Now I know she’s actually joined college so that’s probably the biggest success.
Claire's story
My name is Claire. I was a support worker with vulnerable adults and I have been in the care sector for about 16 years. It’s something I really enjoy.
I supported an individual for several years and we just plodded along. We are supposed to review care plans but people just kept skipping over it. This individual kept showing challenging behaviours so I decided to go through her care plan - go right back, look right into it and see what was happening. I found out that she used to go swimming three times a week, and when she did she had no behaviour reports. But recently she hadn’t been going swimming at all. I couldn’t understand what was happening. I said, ‘Right, we’re going to go swimming so, let's go.’ So, I took her swimming.
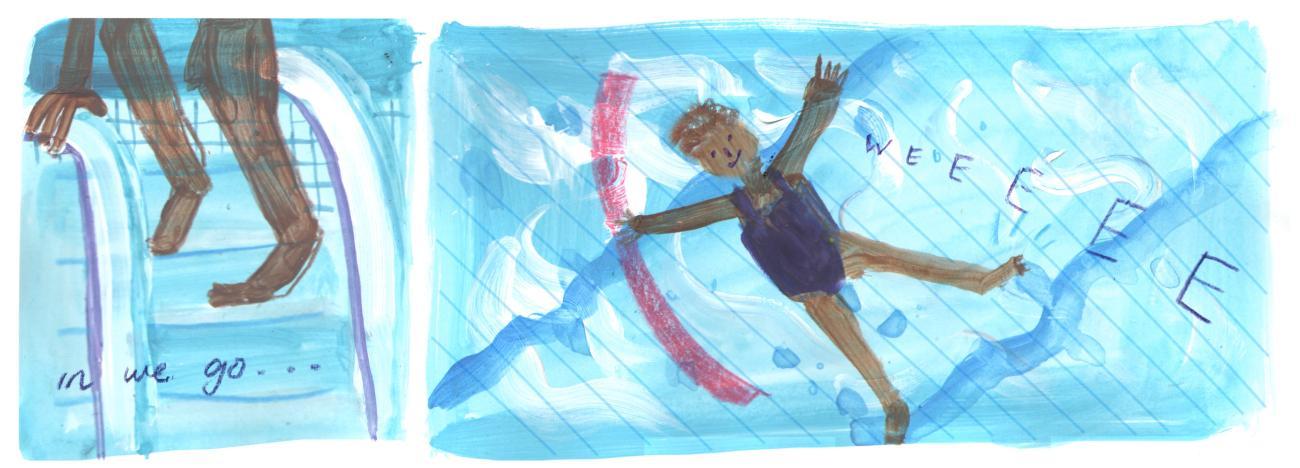
She was non-verbal, she’s 50 years old. We went to the swimming pool and I had to sing her a wee song to get her in - one foot in and then get the next foot in. I got some odd looks from the lifeguards cos I don’t think my singing is very good. We had a wee jig and we got into the water. Then she - it still brings me to tears - put her feet on the side of the pool and she said, ‘Wheee!’ and she went along and honestly that was the first time I’d ever heard her speak.
I was just like, ‘I can’t believe this, I cannot believe this.’ And so, I literally spent about 15 minutes just listening to her say, ‘Wheee! Wheee! Wheee!’ and I was like, tears down my face.
Honestly that lifeguard must have thought there was something really odd about me but it was the most rewarding experience I’ve ever had. Eventually I had to try and get her back out which was a challenge, but we got there and it was absolutely brilliant. She came back and she was so calm. It was really, really good.
I went in to work and said to the manager, ‘Right, why has this not been dealt with? Let’s do this and let’s put it in her care plan.’ There was so much resistance and I couldn’t understand why. I was quite upset, I was quite angry and frustrated. Why were they not listening to her, not listening to this person’s needs? I said to the manager, ‘Look we need to have a discussion with her key workers, we need to try and do this. Even if we could do this once a week. It’s a big massive benefit.’ But all the workers said, ‘Nope, nope, nope we’re not going.’ I couldn’t fathom it.
Eventually we did have a meeting and I spoke to them and they told me their concerns. Some women were concerned as they didn’t want to be in the pool with their swimming costumes on. I could relate to that so I said, ‘It makes me uncomfortable but for the benefit of this individual that little bit of uncomfortableness would make a massive difference.’ And then another one said that once she had done the toilet in the swimming pool and they were extremely embarrassed and they were never taking her back. I was like, okay, so it’s issues of staff embarrassment - we weren’t really meeting this individual’s needs because of our fears. So we all collaborated and decided that if I went along and someone came with me, they could shadow me at the pool and then we could see how that would work. So that’s what we did. I put swimming in place three times a week and she is, as far as I know, doing quite well and that’s still part of her plan. It’s transformed her life.
She’d been in an institution most of her life and then she’d been trying to adapt to being in her own home and now she loves it. She’s enjoying having a new couch and decorating her house and it’s little things that you could pick up on. If she wanted to do something, she would come and touch your nose and if she was hungry she would point to her mouth - it was things that you had to try and really listen. You needed to teach her and to tune into what she was needing. I felt that we hadn’t been listening. We were just plodding on and thinking, ‘Oh well she’s displaying these challenging behaviours, och it’s just her.’ We needed to listen to her to see how we could help her make her life better. It just goes to show that behind every behaviour is a reason. It just needs someone to listen and to take the time and recognise that that’s not part of the norm.
I’m not saying that the other staff members couldn’t have done it, they just needed that one person, me to go in and say, ‘Look, I’ve noticed this, let’s try and do something else.’ I was quite capable of taking her myself, but I think I knew her very well and I felt very comfortable. From then on it was two staff members that went swimming with her. We only had certain people, key workers for her and the other staff were a bit scared. I would say, and it kind of relaxed it when they had another person there or they’ve shadowed me to see, ‘Oh, this is how you would do this kind of thing.’ So, she actually gained more key support workers as well. And her challenging behaviour lessened, so the staff members maybe wouldn’t have been so scared to go in. It kind of opened up the team to be able to go in and work with her rather than only certain individuals.
I think one member of staff moved to support another person, but she felt more comfortable somewhere else and that was fine. But the rest of the staff members were actually glad. They were missing out on what this individual was like. She was so funny and you didn’t notice that unless you actually got to know her, and so there was quite a lot of the other staff members who actually got to know her a bit as well. I enjoyed that.
What I learned from this was that you need to stand up for individuals, you need to give them a voice if they don’t have one and even if it is uncomfortable for you. You feel like you still need to be there for them, you still need to give them a voice cos they need to be heard and that’s what I learned from it.
And listening and resilience and everything, now that I’ve looked at that. I’ve said, ‘I’ve got those leadership qualities, I’ve done that.’ And then you look at it and you can link it to what you’ve actually done, and you think, ‘Oh, wow.’ Cos if somebody tells you that, you think, ‘Oh, that’s really good.’ But then when you start to link it to what we’re doing now. Aye, I felt quite proud of myself sometimes.
I’ve found with some of the units in this course too... like see some of the things that you do within your wee team at work or whatever, you just do it, it’s second nature to you and you don’t realise the impact that it has on your team. It’s second nature, nobody asks you, it’s just what you do. It’s just you.
It just makes you think in my future practice, I’m going to stop and think, ‘Right, why is this happening? Can we figure out what’s going on.’ So, one incident can have a massive impact on everybody.
Carolann's story
I’ve worked in the care sector for roughly five years doing various things such as volunteering at the hospital and various placements through college. I finally got a job three years ago in January with a company to support individuals mostly with learning disabilities out in the community within their own accommodation. That was my first real job in this sector.
I’ll be honest, I didn’t know what to expect and I didn’t know my skills so it was just a case of you got your training and you were left to it! I’m one-on-one with the client.
I started with this person roughly the same age as me, a very independent, smart person. He had been to college himself but it was a situation where he would show interest for so long and then he would be like: ‘No, that doesn’t interest me anymore.’ So, he was kind of always leaving different courses and things.
He had been with the company for roughly about six months before I got allocated to work with him and the consensus of the team was ‘challenging behaviours.’ He doesn’t respect the staff and was always asking them to leave early. I was obviously very anxious and worried about it. I thought ‘what I’m going into here’ especially not really feeling confident at that time cos I was only six months in the role.
When I entered the person’s house it was very messy and he just sat at his computer constantly. There was no communication, no interaction whatsoever. We were there to help him clean his house, to make sure he’s living safely, and to assist with nutritional things like making him cook healthy meals rather than using ready meals all the time, or going to the takeaway which was his common thing at night. We were also there to see what his niche was, what his interests were in order to get him out and be healthy and associate with the community; to get him into clubs and things to get friends. His parents did stay nearby but he was at the age where he wanted to move out and have that bit of independence.
He’s now 35. At the time when I went in he was 32. He had actually came from a previous care company and his parents decided that he was coming to us because again, they were experiencing challenging behaviours with him. I think because it was all new to him, living alone with these random people coming in to try and tell him how to live his life, he was just rebelling against it. He was obviously asking people to leave thinking, ‘Well this is my house, this is what I want: my independence.’
But he didn’t realise we were there to support rather than dictate to him, so when I went in, the first couple of shifts were very challenging just trying to get any communication with him. I looked back at all the case notes to see what everybody wrote. It was the same consensus, ‘He’s asked me to leave.’ But the case notes were very short, so you weren’t getting any detail. Was he shouting? Was he throwing things? Did he speak at all that shift? Did he eat? There was none of that. It was just constantly like, ‘Arrived and asked to leave 10 minutes later.’ And that was it - it was basically starting from scratch.
I realised I could forget about the mess of the house and just try and build rapport from scratch. Let’s just get to know what his interests are. ‘Oh, well you’re interested in cycling? I like cycling. You know someday, I’ll maybe bring my bike to work and we could maybe go and just have a wee cycle. We don’t need to clean the mess; the mess will still be there next week: we’ll get to that.’ It was just building the relationship up.
Within a couple of weeks I had his house, with him, spotless. He realised that he did like doing housework so, it was a case of the partnership working. If I was to go in there and say, ‘Come on, you need to hoover this’ he wouldn’t do it. He would rebel straight away, whereas, if I said, ‘Right, how about I do the hoovering and you do the mopping today or what do you fancy? Do you want to do it the other way?’, he liked the partnership working and not being told what to do. Even though he was more than capable of cleaning his house himself, he just liked that wee bit of help.
The previous staff were going in and basically saying, ‘Come on, look at this mess: we need to clean this.’ And he was kind of feeling as if, ‘They’re telling me to do that, they’re not actually here to help.’ So there was that bit of resistance. Within a matter of weeks we had him cooking healthy meals from scratch which was fantastic. Even making batch meals that he could freeze for the rest of the time - it was just a case of heating them up himself when we weren’t there.
He’s got a keen interest in his computer so sometimes the fire alarm would be going on cos he’s left something on the stove. So it was just getting him to that level of, ‘You need to set timers. Right, I know you’ve set your cooker timer but let’s do it on your phone as well.’ And just that kind of visual reminder, ‘Oh right, my alarm is going off.’ Because if he’s in the other room he would just forget. He can hear the beeping but would just totally ignore it cos he’s too engrossed in the computer.
Within about a year we had joined a gym, which we found out that he loves, so we upped his hours on a Wednesday to take him out to the gym. He was finding it was all exercise and he kind of clicked on to that and he was like, ‘Mmm I’m not really getting anything else here.’ So, we decided, ‘Right, well what do you want to do?’ ‘Well, how about I do the gym every second week and then the weeks in between I’ll do something like the cinema, or I’ll go out for a treat for lunch to Pizza Hut or whatever.’ So, it was just basically working with him and seeing what he actually wanted.
After that my manager obviously realised the change cos she wasn’t getting the phone calls saying, ‘Oh, difficult behaviour and I’ve been asked to leave.’ So, she was like, ‘Are you still there?’ and I’m like, ‘Yeah, I’m still here. I’m 10 minutes over my shift but it’s alright, we’re just finishing off.’ And then it was like, ‘What have you done?’ and straight away I was like, ‘Oh no.’ feeling I’ve overstepped the mark here, like this shouldn’t be me doing this. As soon as that manager says, ‘Come in for a meeting.’ I thought, ‘Oh no, I’m sacked. I’ve no been doing my job.’ So, I was obviously very worried about that but as soon as she says, “No, but how have you managed to do that?”
But then I quickly realised it was a case of, ‘How did you do that? How can we get the other staff in there to do that?’ I asked him, ‘Would you mind if we get the staff members back in and I can sit here and shadow and see where we’re going wrong?” So, it was just that kind of partnership working and making sure like staff members weren’t going in and dictating and saying, ‘Come on, we need to do this. We’ve only got an hour.’ And constantly looking at their watches and that, just taking the time and saying, ‘Aye, we can sit and chat for the first half an hour and then we’ll get the cleaning, there’s no rush.’ And letting him make his decisions in his own house.
And just show him that, ‘I’m still here, I’m not just taking the back seat and it’s going to go back to square one where you feel that way again.’ And just showing him, ‘Well you tell them.’ Rather than me sitting saying, ‘Well, this is how we do it.’ I was like, ‘Well, how do we do it, what normally happens?’ and ‘What would you like to do first, you tell them, you communicate.’ And it went pretty well, so it did.
(The staff) were open to coming back because they couldn’t believe the drastic change. Luckily enough they were able to create the bond that I’d created with him. There wasn’t that resistance anymore and going out after the first couple of shadowing shifts, they were like: ‘That’s a totally different person, that’s no the person we met last year.’ And I said, ‘It’s just that, getting to know them individually rather than going in there and thinking you’re task orientated, like I’ve got to go here and I’ve got to clean up, that’s my duties, that’s what I’m employed to do.’ No, you’re not, you’re there for that service user, you’re there for what they want and what their wishes are. If it means that you’re only in that hour shift and all it is, you’re sitting talking to them one-on-one about how they feel that day, that’s tough, the cleaning will get done another day.
Because I started getting to know him really well, I got introduced to his mother so I was talking to her as well and I was just saying like, ‘Well, I’m not going to clean the house. At the end of the day, support workers aren’t there as cleaners. If you’re wanting a cleaner in, you’re going to have to go above and beyond that. I’m there to support his needs and his wishes and right now the thing about nutritional intake and getting him out the house to activities and making him feel confident, that’s my key goals, no the cleaning.’ I was like that, don’t get me wrong, sometimes I would be over my shift because I’d go in there and be like, ‘Oh toilet. I’ll clean the toilet, can’t leave that’. Typical mother head but other than that, no, if there was piles of clothes everywhere, I’d be like, ‘We’ll get them next week.’ He’ll soon realise he’s no got any clean clothes and we’ll need to do a washing and his mum was constantly going in and she was picking up the slack of the cleaning. But she was quite happy with the way I was working it, so no I’m happy now because … I’m still in contact with him and just seeing how happy and confident he is and now he travels independently up to Glasgow and things so he’s a totally changed person.
So, we spent a good few months doing that and within 18 months he didn’t need the service anymore. He was confident enough to say, ‘No, it’s alright I don’t need you. I can cook, I can clean, I know how to clean my house. I know the products to use.’ And the amount of groups he’s joined. He’s back at college now, and as far as I’ve heard from his mother, is now doing a computing course.
I’m still in the same role. Now I’m more focussed on my studies but I would like to think it’s increased my confidence for other service users. I’m no as shy thinking, ‘Oh no, I should be in here task orientated and I’m in here to make a meal and give medication.’ I am more a case of, ‘No, I’ll sit and talk to the person and we’ll get the medication at the end, we’ll be fine.’
I just think it’s looking at the bigger picture as well ... and you will all be sort of aware of the wider factors that impact on the commissioning and procurement of care services and some of the formulas that go around like, you’ve got 15 minutes with this client and 12 minutes with that client and you’ve got to get from A to B and B to Z and all the rest of it. How do you count your time?
Because of this process we’ve actually now introduced a match-making service for when you’re hiring the individual - matching the interest to the service user. Having that initial link straight away rather than just putting any worker with any service user. We have started inviting the service users to the interview process for them to meet the person straight away, to get that initial, ‘Do I like you, do I not?’ and for them to ask questions that are obviously important to them. So, there’s been two big changes as well in the company.
Jenna's story
I have always been interested in social care. I’m a care experienced young person/adult. Having come through the care system I realised quite early on that I wanted to be involved in the care sector to change things because I didn’t like my experience with professionals in the care system. I thought they were anything but professional. That was why I kind of went on my journey through social care, did my HNC and then I ended up here. I’m still not sure exactly where I want to go and that was why I chose this course because it opens up more doors rather than a social work degree and then you’re a social worker.
I was a community support worker, working with adults with learning, physical and mental health issues in the community. The person I was supporting had a diagnosis of Parkinson’s and Multiple Sclerosis. He was bed bound.
One day I arrived with my colleague for morning support and the door was unlocked which was very unusual; his wife usually let everybody in. The guy was always usually cheery, although he was bed bound, he was still quite a happy-go-lucky guy. Previously he’d been in the army, but due to his condition, mental health was quite a big thing. You find with people that are bed bound that they get quite depressed because they can’t really do anything.
I went in that morning and he was crying and wasn’t good. I asked him what was up and he told us that his wife had left him. So, initially I was quite sad. Obviously the breakdown of any relationship is quite sad, nevermind the fact that he can’t do anything about the situation. So, I contacted the boss to inform them of the situation but her phone was off; she was in a meeting. I called social services to get his social worker; she wasn’t in the office. I was asked if I wanted to leave a message and told them it was quite important. They said that she was going on holiday after that day for a fortnight. Now, having experience with social work, you don’t … 90% of the time, you don’t get a response that day, it’s two or three days later that you get a response from them.
My first thought was that he doesn’t have a lock on the front door and he lives on the main street. It’s a busy road - the main road through the village. I mean everywhere’s the same, drugs are a massive issue within every community. He had a diagnosis of Multiple Sclerosis and Parkinson’s and used controlled drugs, which had street value so they needed to be locked away. As they are of use to people with addictions it was very worrying. Initially I was like, ‘Oh no’ but you just do what you’ve got to do.
I was pacing about his house like nothing else. The poor guy and obviously he’s bed-bound so, that was probably making his anxiety 110 times worse because I’m in and out and he’s only hearing bits of conversations. It was about him - he’s got the right to hear every single thing that I’m saying on that phone and probably for me to put the phone on loud speaker to hear the response too. But I was in a heightened state - I never had anything like this happen before. I’d never dealt with anybody’s wife leaving them, never mind in my job, if you know what I mean? So my anxiety was through the roof and I was pacing about the floor and that’s probably the main thing that I would have changed about the situation - I would have stayed in the room beside him and let him hear everything that was happening.
I did start to panic - it was manic. We’re only supposed to be there for an hour in the morning. It was a single at lunch time and then a double up at night time again, so I had other services to go to. We were social support mainly, so we were like three hours, five hours … I think the 15-minute visits should be totally done away with but there you go. So, aye so, that was my situation. I phoned my boss and asked if I could stay while my colleague would obviously pick up my other services and that was fine. Aye, well that company were alright at things like that. They were very much supportive of the support worker because you’re in there, every day.
I mean what else were you supposed to do? Well, I mean social services were quite happy for me to walk away from that service and leave that door open. I couldn’t have gone to my bed that night knowing fine well on a Friday night that there’s folk walking by that house kenning that the front door is open. If somebody walks in there, that guy can’t do anything, he’s bed-bound, he couldn’t … there’s nothing he could do. Press his community alarm, community alarms going to ring through, ask him what’s wrong. Do you know what I mean? If somebody is there threatening them, ‘Tell them that everything’s fine.’ Oh, everything goes through my head.
So, I took it upon myself to get a key safe, a money box and a locked cupboard for his medication. I phoned my boss to get permission and she said that it was fine. I bought a key safe and a money box.
Aye, see it’s not down to the care company to install the key safe, it’s actually down to the family but he didn’t have any family other than his wife. So, I took it upon myself … I asked for the money, he paid for it, and the only person available to fit it that I knew of was my partner. My boyfriend’s no exactly the best DIY’er but we’ve got a drill. I knew through being in the care sector you know the way, well a key safe, it’s not that hard to fit. It’s just two rawl plugs into the wall and two screws but you need a drill. So, I phoned him, and I was like, “will you come and aye, help me.” And he did, he knew cos we’re from the village, well he’s from the village that I was working in so, he knew the guy (he had fixed a couple of my boyfriend’s cars) so he came and fitted the key safe, and it was the individual that picked the number.
We installed it on the wall outside, down by the stairs so that it wasn’t visible from the main street and folk couldn’t see, ‘Oh, there’s a key safe.’ So it doesn’t make him more vulnerable. Aye.
So, I got the key safe, got it fitted, and informed social services, the boss and community alarms. The same with the locked cupboard for the medication and then a money tin as well to put all his money in and a receipt book. It wasn’t really a receipt book, just an A4 bit of paper, but I had to do something cos you’ve got to monitor everything and it was just a case of gathering all the money that was in the house, counting it, putting it in the tin and just starting a sheet. What you took out, what you put back in, with receipts and that was it.
Although he was sad, I gave him a big cuddle before I went and he was like, ‘Thanks for the day, thanks for everything.’ But I could walk away knowing that aye, he’s going to be sad cos his wife’s left and that happens in life, but you don’t get left in that situation. No everybody’s as unfortunate not to have any family, ken what I mean? So, aye when I walked away it was probably the best feeling ever.
I knew that he was safe, he’d had all his medication and he would be fine until the next morning. I was his main support worker.
Some people would just leave it at that - ‘Well I’ve notified such and such and passed it onto someone.’ And go, ‘Well they don’t have this, they don’t have that, but I’ve got to go to someone else.’ There are people that would actually do that. I just couldn’t. Aye, I was anxious. I was nervous. I was sad. I was everything but walking away, locking the door and putting the key in the key safe, I felt amazing because I knew that he was quite happy with how I’d helped. You just get days like that sometimes, don’t you? But again, it wasn’t until I did this that I actually realised that I done anything … above and beyond.